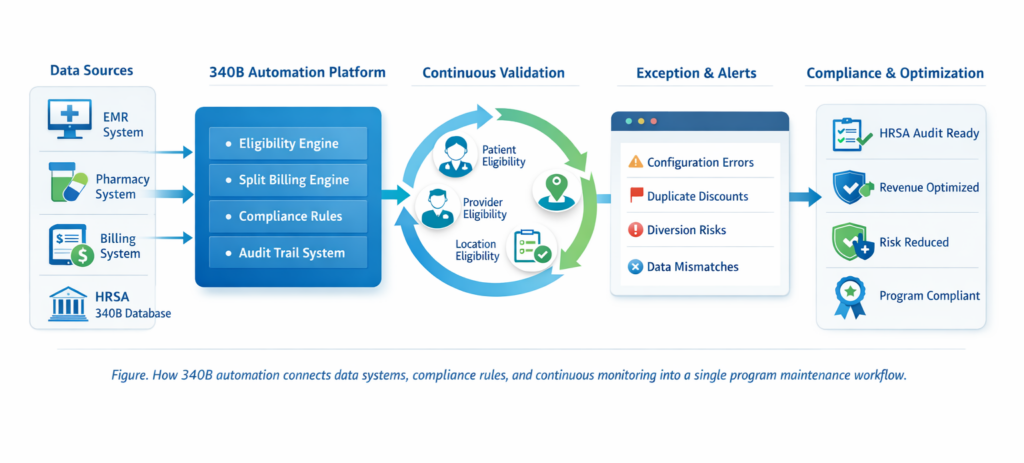
340B automation is the use of technology to monitor and protect how discounted drugs are applied under the 340B program. It ensures only eligible patients, providers, and locations receive 340B pricing while enforcing HRSA rules automatically.
Modern healthcare systems handle thousands of prescriptions daily across EMR, pharmacy, and billing platforms. Without automation, disconnected systems create gaps that can lead to diversion, duplicate discounts, and audit failures.
Automation maintenance applies compliance rules in real time, validating each claim before it becomes a financial or regulatory risk. This shifts 340B from reactive oversight to continuous control, protecting revenue, ensuring audit readiness, and enabling safe 340B optimization.
Why This Workflow Matters?
This visual explains something that auditors, executives, and compliance officers all care about. It shows that 340B automation is not a reporting tool. It is a live control system. Data does not move freely through the organization. It moves through validation gates. Each gate protects the organization from diversion, duplicate discounts, and audit failure. This is what converts automation into a true 340B program compliance infrastructure.
What Is 340B Automation and Why Is It Important?
340B automation refers to the use of connected software systems that apply HRSA rules, eligibility logic, and billing validation automatically across EMR, pharmacy, and revenue cycle platforms. Instead of relying on humans to remember policies, automation converts those policies into enforceable system logic. That means eligibility is not something that is reviewed later. It is something that is enforced at the time of care and at the time of billing.
This matters because the 340B program is dynamic, with providers, locations, and payer rules constantly changing.. Providers change locations. Clinics open and close. Medicaid carve-in status changes. Contract pharmacies come and go. When these changes are not reflected instantly inside billing systems, compliance breaks. Process automation eliminates that risk by synchronizing all systems with one compliance brain. 340B program compliance becomes a permanent operating condition rather than a quarterly scramble.
Why Manual 340B Maintenance Is No Longer Sufficient
Manual maintenance fails because it depends on static snapshots in a real-time environment. A provider may become ineligible today, but the billing team might not update their spreadsheet until next month. During that time, every claim attached to that provider becomes a potential audit violation. Multiply that risk across hundreds of providers, multiple locations, and dozens of contract pharmacies and the exposure becomes massive.
Without automation maintenance, healthcare organizations unknowingly accumulate compliance debt. By the time a discrepancy is discovered, claims have already been submitted, discounts have already been taken, and repayment obligations have already been created. 340B automation changes that model by stopping errors before they ever enter the financial system.
How Does Automation Improve 340B Compliance Outcomes?
When 340B automation is deployed, compliance is enforced through technology rather than memory. Every transaction is checked against current eligibility rules before it is allowed to proceed. This shifts the entire risk profile of a 340B program. Instead of detecting problems later, organizations prevent them from happening.
How Automation Strengthens Compliance Controls
- Real-time patient eligibility validation
- Provider and site verification before claim processing
- Duplicate discount detection at the transaction level
- Automated audit trail creation
These controls operate continuously, which means 340B compliance is not something that can drift quietly over time.
How Data Governance Supports 340B Automation
340B automation is only as reliable as the data it uses. Data governance ensures that patient records, provider files, drug databases, and payer information are accurate, current, and synchronized. Without strong governance, even the best automation platform can produce incorrect eligibility decisions. This is why enterprise healthcare systems treat 340B program compliance as a data management discipline as much as a regulatory one.
When governance policies define how data is created, updated, and validated across systems, automation maintenance becomes stable and predictable. This prevents silent data corruption, which is one of the most dangerous risks in 340B programs.
What Role Does Automation Play in Continuous 340B Maintenance?
Automation maintenance ensures that compliance does not depend on manual updates. When a provider leaves a covered entity, the system knows immediately. When a clinic loses eligibility, billing logic adjusts automatically. When a payer changes its carve-in policy, the rules update across all claims. This creates a closed loop system where no data change goes unvalidated.
Continuous maintenance is what allows organizations to survive audits. HRSA no longer evaluates just outcomes. They evaluate processes. A system that continuously enforces rules is defensible. A spreadsheet updated once a month is not.
How Automation Reduces Diversion and Duplicate Discounts
Diversion occurs when drugs are dispensed to ineligible patients. Duplicate discounts occur when Medicaid rebates and 340B discounts are both applied to the same drug. These are not malicious errors. They are data failures. 340B automation prevents both by verifying every required element before a discount is allowed.
The system checks patient eligibility, provider eligibility, location eligibility, and payer status simultaneously. If any element is invalid, the claim is blocked from 340B pricing. This real-time enforcement is far more effective than any retrospective audit.
How Contract Pharmacies Fit into 340B Automation
Contract pharmacies significantly increase 340B risk because they operate outside the covered entity’s internal systems. 340B automation extends compliance controls into these external environments by validating every transaction before a discount is applied. This ensures that third-party dispensing still follows the same rules as internal pharmacies.
By centralizing contract pharmacy data into the same compliance engine, organizations maintain full visibility, consistent enforcement, and audit-ready documentation. This is essential for 340B program compliance in networks that rely heavily on retail pharmacy partnerships.
What Are the Key Components of Automation Maintenance in 340B Programs?
- Eligibility engines that validate patients, providers, and locations
- System integration between EMR, pharmacy, and billing platforms
- Automated audit trail and documentation generation
- Exception monitoring and configuration tracking
These components together create the backbone of 340B automation.
How Automation Enhances Audit Readiness
HRSA audits focus on documentation, traceability, and consistency. 340B automation provides all three. Every transaction is recorded with timestamps, eligibility checks, and applied rules. This creates a digital chain of custody for every discounted prescription.
When auditors ask how a claim qualifies, the answer is already documented. This dramatically reduces financial risk, repayment exposure, and operational disruption.
How Automation Improves Operational Efficiency
Automation reduces manual workload, allowing teams to focus on high-value tasks rather than repetitive compliance checks. By automating daily monitoring and validation, operational efficiency improves.
Organizations using process automation see:
- Fewer manual data reviews
- Faster resolution of discrepancies
- Improved coordination across departments
- Reduced administrative costs
Efficiency gains allow staff to focus on program optimization while maintaining strong 340B program compliance.
How Automation Enhances Accuracy in Split Billing and Data Mapping
Split billing depends on perfect data alignment between drug codes, charge masters, and eligibility files. Manual updates cannot keep pace with constant code changes. 340B automation continuously reconciles these data sets and alerts teams when mismatches occur. This prevents pricing errors and compliance breaches before money moves.
How Automation Supports 340B Optimization Beyond Compliance
Automation not only ensures compliance but also enables 340B optimization. Accurate, real-time data allows organizations to maximize eligible claims, manage inventory, and forecast revenue.
340B automation helps:
- Capture all eligible claims accurately
- Optimize inventory and resource allocation
- Improve financial forecasting
- Reduce revenue leakage
With automated compliance, healthcare organizations can safely pursue optimization opportunities without risking program integrity.
How Automation Protects 340B Revenue Integrity
Revenue integrity is not just about collecting money. It is about collecting the right money under the right rules. 340B automation ensures that no eligible prescription is missed and no ineligible prescription is discounted. This protects both top line revenue and regulatory compliance.
When process automation governs pricing decisions, organizations eliminate under-capture and over-discounting. This balance is what allows 340B optimization to occur without triggering audit risk.
Real World Use Cases of 340B Automation
- Large hospital networks validating thousands of providers across hundreds of sites
- Contract pharmacy networks governed by centralized compliance engines
- Health systems preventing millions in repayment exposure through real time validation
- Compliance teams moving from quarterly audits to continuous assurance
These outcomes are only possible with automation maintenance.
How Should Healthcare Organizations Approach 340B Automation Implementation?
Successful implementation begins with mapping current workflows, identifying risk points, and integrating all systems into one compliance platform. Training ensures staff can manage exceptions while automation handles routine validation. Over time, rules are refined based on performance data, creating a living compliance engine.
340B Automation Implementation Table
| Flow Stage | Data Source | Automation Action | Compliance Purpose | Business Impact |
| Patient Encounter | EMR | Patient eligibility validated in real time | Prevents diversion | Protects program integrity |
| Provider Assignment | EMR Credentialing | Provider and location verified | Ensures eligible prescribers | Avoids audit violations |
| Prescription Dispense | Pharmacy System | NDC and drug eligibility checked | Validates covered outpatient drugs | Prevents ineligible discounts |
| Claim Creation | Billing System | Payer and Medicaid status verified | Prevents duplicate discounts | Protects revenue |
| Pricing Decision | 340B Engine | Discount applied or blocked | Enforces HRSA rules | Eliminates compliance risk |
| Documentation | Audit Engine | Full audit trail stored | Proves compliance | Supports HRSA audits |
| Reporting | Compliance Dashboard | Exceptions and trends analyzed | Enables governance | Supports optimization |
Who Owns Compliance in an Automated 340B Environment
Automation does not remove accountability. It clarifies it. In modern 340B programs, compliance ownership is shared between compliance officers, pharmacy leadership, revenue cycle teams, and IT governance. 340B automation provides a single compliance truth that all departments rely on.
This shared visibility ensures that automation maintenance is transparent and defensible, which is a critical requirement for HRSA auditors.
Challenges When Adopting 340B Automation
While automation is powerful, organizations must address potential challenges:
- Ensuring high data quality
- Managing complex system integrations
- Overcoming resistance to change
- Avoiding over-reliance on technology
- Managing initial investment costs
Addressing these challenges ensures 340B automation strengthens program compliance rather than creating new risks.
Why Cybersecurity and IT Integration Matter for 340B Automation
Because 340B automation connects EMR, pharmacy, and billing systems, it becomes part of the organization’s critical IT infrastructure. Security, access control, and system reliability directly impact 340B program compliance. Unauthorized changes or data breaches can create false eligibility or pricing errors.
For this reason, leading healthcare systems treat 340B automation platforms as regulated financial systems, not just compliance tools.
Future Trends in 340B Compliance with Automation
The future of 340B compliance is continuous, technology-driven, and data-focused. Emerging trends include:
- Real-time compliance analytics
- Predictive risk detection
- AI-assisted audits
- Enhanced system interoperability
- Increased regulatory transparency
Healthcare organizations adopting 340B automation today will be well-positioned to meet future regulatory requirements.
Conclusion
340B automation transforms program maintenance and compliance outcomes. It shifts programs from reactive, manual oversight to continuous monitoring. Organizations that embrace automation maintenance maintain stronger 340B program compliance, optimize operational efficiency, and maximize program value through 340B optimization. In an environment of evolving regulations and growing complexity, 340B automation is essential for sustainable, efficient, and compliant healthcare operations.
Frequently Asked Questions
What is 340B automation?
340B automation is the use of connected technology systems that continuously manage patient eligibility, provider relationships, pharmacy dispensing, and billing rules so that only qualified prescriptions receive 340B pricing.
Is automation required for 340B compliance?
Automation is not legally required, but automation maintenance is considered best practice for protecting 340B program compliance. HRSA expects covered entities to have systems capable of preventing errors, not just detecting them.
Can automation eliminate all compliance risk?
No system can remove all risk, but 340B automation eliminates the most common causes of violations such as data mismatches, provider eligibility drift, and payer misclassification.
How does automation help during HRSA audits?
Automated systems generate timestamped audit trails that show exactly how eligibility was determined for each prescription. This makes audits faster, cleaner, and far less risky.
Does automation replace 340B specialists?
No. It allows specialists to stop doing manual checking and focus on governance, oversight, and 340B optimization.
Is 340B automation suitable for small programs?
Yes. Even small covered entities face the same compliance rules and the same financial penalties. Automation maintenance is often more valuable for smaller teams because it prevents mistakes they cannot afford.